In This Issue
- 4th Quarter Benefit News Highlights
- FEATURE: One Big Beautiful Bill Act (OBBBA)
- FEATURE: 2026 Federal Compliance Calendar
- FEATURE: Benefits During an Unprotected Leave of Absence
4th Quarter Benefit News Highlights
1 – ICHRA Affordability – Updated Premium Look-Up Table
The affordability of an ICHRA is tied to the lowest cost silver plan available on the public Exchange/Marketplace. The rates vary based on an employee’s worksite or residence, so CMS publishes premium data via a Look-Up Table for Federally-facilitated Exchanges and State-based Exchanges using the Federal Platform. Employers can use this information to help determine affordability for their ICHRA offering. Plan year data for 2019 – 2026 can be found here – Employer Initiatives | CMS
2 – Trump Accounts – IRS Guidance
IRS Notice 2025-68 announces the IRS’s intent to issue proposed regulations implementing Trump Accounts (TAs)—a new type of IRA added under the One Big Beautiful Bill Act (OBBBA) that may be established for eligible minors. The notice provides some initial guidance on how these accounts will operate. Beginning July 4, 2026, employers may contribute up to $2,500 per year (indexed annually) per employee on a tax-favored basis via Trump Account Contribution Plans (TACPs). The notice also confirms that TACPs may be offered through cafeteria plan salary reductions, and that further rules coordinating TACPs with cafeteria plans will be addressed in upcoming proposed regulations. The notice can be found here – Notice of intent to issue regulations with respect to section 530A Trump accounts
3 – Reminder – Gag Clause Attestation Due Soon
CMS sent out a reminder email for gag clause attestations, which are due annually by December 31. The reminder provides a short set of FAQs for the annual attestation requirement. It also describes the minor changes made to the attestation form and process for 2025. You can find the email here – Reminder to submit your annual Gag Clause Prohibition Compliance Attestation
Carriers will generally handle the attestation on behalf of fully-insured group health plans. Service providers (e.g., TPAs and PBMs) may handle the attestation on behalf of self-funded group health plans, but otherwise the employer is responsible to attest. For employers looking for a vendor to handle the attestation, see Lumelight’s solution here – Gag Clause Compliance – Lumelight
4 – CMS Final Rule – Hospital Pricing Transparency
CMS’s recent final rule aims to strengthen hospital price transparency requirements beginning in 2026. Hospitals must publicly disclose actual (rather than estimated) allowed amounts along with counts and National Provider Identifiers (NPIs) in machine readable files (MRFs), backed by a formal accuracy attestation. While this could certainly increase price transparency, the required MRFs remain highly technical and difficult for the average consumer to interpret. As a result, employers and third-party tools will play a critical role in translating these data into usable insights for plan members. That being said, more accurate, transparent pricing data may give employer-sponsored group health plans stronger leverage in evaluating hospital contracting and benchmarking provider prices. Employers might also use the information to enhance benefit design strategies such as tiered networks, reference pricing, and steering toward lower-cost care settings. The fact sheet for the final rule can be found here – CY 2026 OPPS and Ambulatory Surgical Center Final Rule – Hospital Price Transparency Policy Changes | CMS
5 – Guidance for Electronic Submission of ACA Employer Reporting
The IRS has released Publication 5164 and 5165 for the 2025 filing season, providing updated guidance for electronic submission of Forms 1094 and 1095 through the AIR system. While the publications outline technical standards and testing procedures, most employers will continue to rely on third-party vendors for electronic reporting due to the complexity of obtaining a Transmitter Control Code (TCC), meeting formatting specifications, and completing required testing. Employers should confirm they are prepared to electronically file or have a vendor solution in place ahead of the 2025 reporting deadlines. The publications can be found here – Publication 5164 (Rev. 10-2025) and here – Publication 5165 (Rev. 12-2025)
For information about Lumelight’s ACA Employer Reporting solutions, see here – ACA Reporting – Lumelight
6 – Kaiser Family Foundation (KFF) Survey
The 2025 KFF Employer Health Benefits Survey underscores the continued rise in employer-sponsored health costs, with family premiums climbing 6% to nearly $27,000 this year. Employees are contributing roughly $6,850 on average toward that total, reflecting the sustained pressure both workers and employers face in managing healthcare expenses. Beyond premiums, cost-sharing burdens continue to climb. The average deductible for single coverage rose to $1,886, with employees at smaller firms facing substantially higher out-of-pocket costs.
Employers cite escalating prescription drug prices—especially for new therapies and weight-loss medications—as a major factor behind rising costs. Chronic disease and hospital costs are also significant drivers. In response, employers are increasingly exploring new care models to improve value and manage costs: nearly a third of firms with 50 or more workers now contract for virtual primary-care services, and some are forming direct arrangements with provider groups.
You can find extensive detail from KFF’s survey here – 2025 Employer Health Benefits Survey | KFF
7 – CMS Marketplace Fact Sheet
While we wait to see whether enhanced advanced premium tax credits, which are set to expire at the end of 2025, will make it into the budget bill currently being negotiated by Congress to end the government shutdown, CMS released a fact sheet outlining its expectations for the 2026 Marketplace plan year. The fact sheet highlights efforts to preserve consumer choice, stabilize premiums, and expand access to HSA–eligible plans. You can find the fact sheet here – Plan Year 2026 Marketplace Plans and Prices Fact Sheet | CMS
8 – FAQs – Fertility Coverage Options
Recent agency FAQs clarify that employers may offer fertility-related benefits (e.g., in-vitro fertilization) as an excepted benefit, provided the coverage is offered under a separate, fully-insured policy and is not coordinated with another group health plan maintained by the same plan sponsor. The benefit would be treated similarly to a specified disease or fixed indemnity policy. Because excepted benefits are exempt from many ACA coverage mandates, they do not need to be integrated with the employer’s major medical plan and do not affect HSA eligibility.
The FAQs further explain that fertility benefits meeting the requirements of §213(d) may also be reimbursed through an Excepted Benefit Health Reimbursement Arrangement (EBHRA). An EBHRA may be offered to employees who are eligible for—though not necessarily enrolled in—the employer’s major medical plan, with annual reimbursement limited to $2,200 for 2026.
Outside of an EBHRA, employers currently cannot offer a stand-alone, self-funded reimbursement arrangement for fertility benefits that would qualify as an excepted benefit. However, the agencies have indicated an intent to pursue rulemaking that could expand how fertility benefits may qualify as “limited excepted benefits,” potentially allowing self-funded options in the future.
The FAQs can be found here – FAQs about Affordable Care Act Implementation Part 72 | U.S. Department of Labor
9 – Employer Plan Sponsor Responsibilities
A federal court in Minnesota (Orrison v. Mayo Clinic) allowed claims to proceed that the plan and its administrator failed to disclose out-of-network reimbursement methodology (a breach of its ERISA fiduciary duties) and failed to maintain an accurate provider directory (a violation of the No Surprises Act/Transparency requirements). This provides a reminder for employers (as plan sponsors) to work with carriers, TPAs, and other vendors to maintain accurate provider directories for participants and ensure plan documents and participant materials clearly explain cost-sharing calculations—especially how allowed amounts for out-of-network services are determined. The court decision can be found here – USCOURTS-mnd-0_24-cv-01124-0.pdf
10 – 2025 Final Form 1094-C & Form 1095-C
The IRS has released the final 2025 Forms 1094-C and 1095-C with no changes from how they looked in 2024. We’re still waiting on the 2025 accompanying instructions, but we don’t anticipate changes there either, so employers can begin preparing now for the upcoming ACA employer reporting season. The forms can be found here – About Form 1094-C, Transmittal of Employer-Provided Health Insurance Offer and Coverage Information Returns | Internal Revenue Service
11 – IRS 2025-2026 Priority Guidance Plan
The IRS released its 2025–2026 Priority Guidance Plan, which outlines the agency’s intended areas of focus for the coming year. For employer-sponsored health and welfare benefits, there are no real surprises in the plan—most of the items listed are routine updates such as the annual release of cost-of-living adjustments, Health Savings Account (HSA) limits, and the Patient-Centered Outcomes Research Institute (PCORI) fee notice. While no major new initiatives affecting health and welfare plan design are included, the plan does provide a helpful indication of when employers can expect the IRS to issue these regular updates. You can find the plan here – 2025-2026 Initial PGP
12 – HIPAA Security Risk Assessment Tool Updated
Employers sponsoring group health plans that are covered entities under HIPAA are required to conduct a security risk analysis for electronic protected health information (ePHI). Employers can use the Security Risk Assessment (SRA) Tool created by the Department of Health & Human Services Office for Civil Rights (OCR) to assist with this analysis. The tool guides organizations in identifying where ePHI is stored or transmitted, evaluating vulnerabilities, and documenting risks with corresponding mitigation steps. The latest version (v3.6) enhances usability with clearer guidance, updated questions and responses that reflect current cybersecurity practices, and improved educational content addressing areas such as encryption and incident response. The latest version of the SRA Tool can be found here – Security Risk Assessment Tool | HealthIT.gov
In addition, find more information about Lumelight’s HIPAA solutions here – HIPAA Privacy & Security – Lumelight
FEATURE: ACA Employer Reporting Summary
Certain employers, plan sponsors, and insurers are required to report health plan information and participant coverage data to the IRS each year. The IRS uses this information to administer and regulate various aspects of the Affordable Care Act (ACA), including an individual’s eligibility for a premium tax credit when purchasing health insurance through a public Marketplace and the §4980H employer shared responsibility rules. Failure to report complete, accurate, timely information can result in significant reporting penalties up to $340/form.
Employer Reporting Responsibilities
Applicable Large Employers (ALEs)
All ALEs (those with at least 50 full-time equivalents (FTEs)) are required to report on offers of coverage to full-time employees. ALE status is determined by averaging FTEs for the previous calendar year. For example, if an employer averaged 50 or more FTEs during 2024 (alone or as part of a larger controlled group or affiliated service group), the employer is an ALE for 2025 and required to report offer of coverage information early in 2026 (for the 2025 calendar year). ALEs report offer of coverage information using Forms 1094-C and 1095-C. Offer of coverage reporting on the “C” forms will never be handled by the carrier but instead must be done by the employer or a vendor on behalf of the employer.
Employers Offering Self-Funded Group Health Plan Coverage
Any size employer who provided self-funded (including level-funded) coverage during 2025 must report coverage information for all individuals enrolled in the plan, including employees, non-employees (e.g., owners, retirees, COBRA participants), and their spouses and dependents. Small employers (<50 FTEs, non-ALEs) report this coverage information using Forms 1094-B and Form 1095-B. ALEs generally report this coverage information in Part III of the Form 1095-C.
Timing of Reporting
Employer reporting is required annually and is done early in the year for the previous calendar year. Reporting is based on calendar year data (even for employers with a non-calendar year medical plan).
2025 Reporting Deadlines
| Form 1095s to employees and covered individuals | Due March 2, 2026 |
| Submission of Form 1094 and all Form 1095s to the IRS | Due March 31, 2026 |
Reporting Method of Delivery
Distribution to Individuals
The options for distribution of Form 1095s are: (i) hand delivery; (ii) mail; (iii) electronically if individuals consent to electronic delivery; or (iv) NEW as of 2024 – post a notice of availability.
| Posting Notice of Availability Distribution to individuals can be satisfied by providing a “clear, conspicuous and accessible notice” that the forms are available upon request. The notice must include an email address, physical address, and telephone number that can be used to request a copy of Form 1095. Notice must be posted on the employer’s public-facing website so that it is accessible to all possible Form 1095 recipients. The notice must be posted by March 2 and remain posted through October 15. If a Form 1095 is requested, it must be provided within 30 days and would have to be hand delivered or mailed unless the employer obtains consent to provide Form 1095 electronically. |
IRS Submission
For almost all employers, Form 1094 and all Form 1095s must be submitted to the IRS electronically.
| Electronic Filing Requirements Employers who file 10 or more tax forms must file electronically (previously only those filing 250 or more forms were required to file electronically). The count includes not only Form 1094 and Form 1095s, but also any other information tax returns the employer may file during the year (e.g., W-2s or 1099s), and therefore, almost all employers will be required to file electronically. This is also true for any corrections that may need to be filed. Most employers use the services of a vendor or reporting software to handle the electronic transmittal to the IRS. |
State Coverage Reporting
A handful of states (CA, MA, NJ and RI) and D.C. have individual coverage mandates requiring residents to have minimum essential coverage or pay a state tax penalty. To enforce these mandates, these states require group health plans, both fully-insured and self-funded, to report coverage information to the states. Employers offering group health plans with covered individuals residing in these states may be required to send reporting to the state tax department in addition to the coverage information submitted to the IRS. In most cases, the same Form 1094 and Form 1095s can be sent to the applicable state tax department to satisfy the reporting requirement. NOTE: Posting notice of availability for Form 1095s as permitted by the IRS may not satisfy state distribution requirements.
Resources
IRS forms and instructions for 2025 reporting (due in early 2026) can be found on the IRS website at:
https://www.irs.gov/forms-pubs/about-form-1095-b
https://www.irs.gov/forms-pubs/about-form-1094-c
https://www.irs.gov/forms-pubs/about-form-1095-c
https://www.irs.gov/forms-pubs/about-form-1094-b
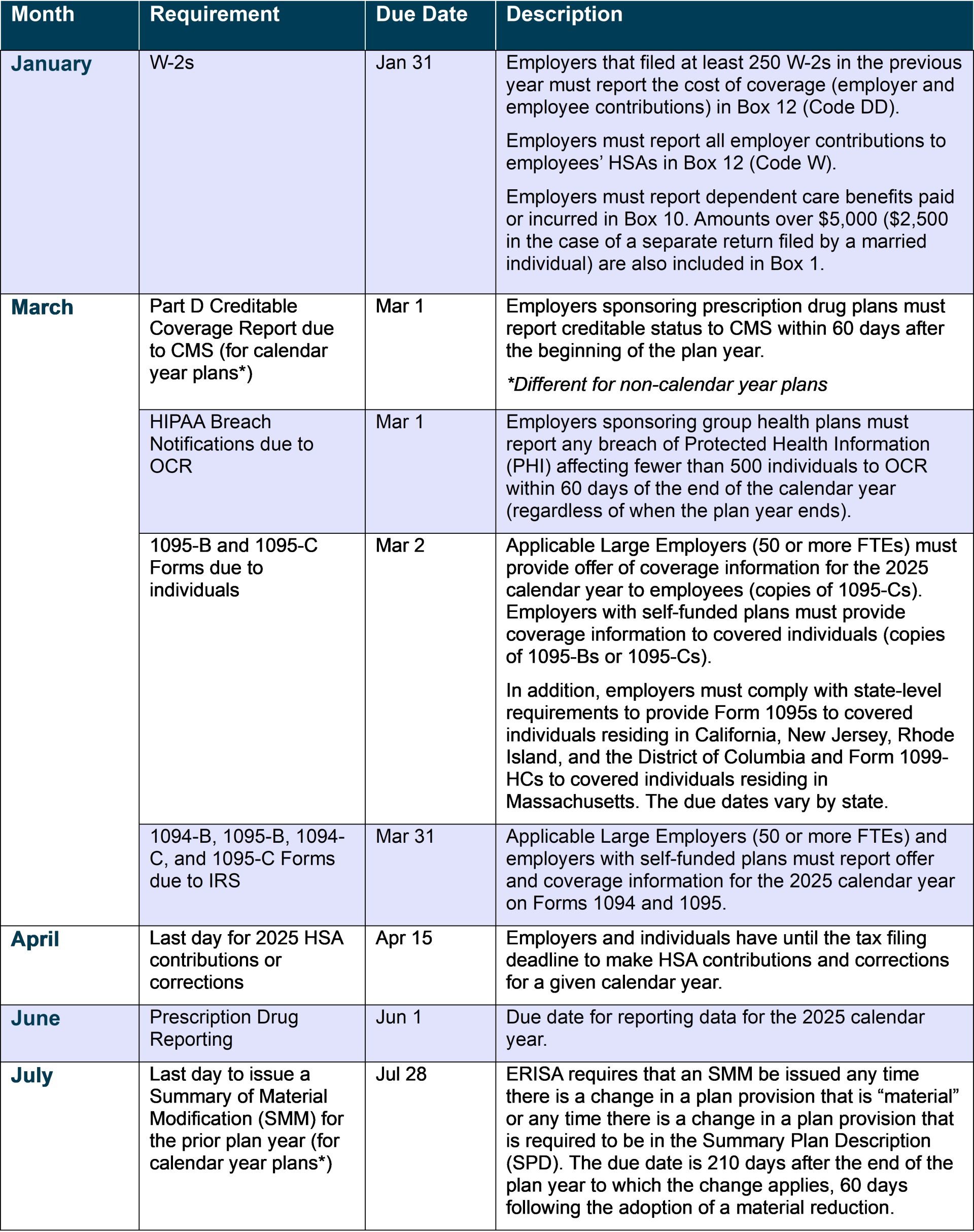
FEATURE: 2026 Federal Compliance Calendar
Due Dates for Non-Calendar Year Plans
Medicare Part D Disclosures (Due 60 days after the start of the plan year)
| Plan Year Beginning | Medicare Part D Creditable Coverage Reporting Due to CMS |
| December 1, 2025 | January 30, 2026 |
| January 1, 2026 | March 2, 2026 |
| February 1, 2026 | April 2, 2026 |
| March 1, 2026 | April 30, 2026 |
| April 1, 2026 | May 31, 2026 |
| May 1, 2026 | June 30, 2026 |
| June 1, 2026 | July 31, 2026 |
| July 1, 2026 | August 30, 2026 |
| August 1, 2026 | September 30, 2026 |
| September 1, 2026 | October 31, 2026 |
| October 1, 2026 | November 30, 2026 |
| November 1, 2026 | December 31, 2026 |
5500 Reporting (Due the last day of the 7th month after the end of the plan year)
| Plan Year Ending | 5500 Due | Due Date with Extension |
| June 30, 2025 | January 31, 2026 | April 15, 2026 |
| July 31, 2025 | February 28, 2026 | May 15, 2026 |
| August 31, 2025 | March 31, 2026 | June 15, 2026 |
| September 30, 2025 | April 30, 2026 | July 15, 2026 |
| October 31, 2025 | May 31, 2026 | August 15, 2026 |
| November 30, 2025 | June 30, 2026 | September 15, 2026 |
| December 31, 2025 | July 31, 2026 | October 15, 2026 |
| January 31, 2026 | August 31, 2026 | November 15, 2026 |
| February 28, 2026 | September 30, 2026 | December 15, 2026 |
| March 31, 2026 | October 31, 2026 | January 15, 2027 |
| April 30, 2026 | November 30, 2026 | February 15, 2027 |
| May 31, 2026 | December 31, 2026 | March 15, 2027 |
Summary of Material Modifications (Due within 210 days after end of plan year)
| Plan Year Ending | SMM Due |
| June 30, 2025 | January 26, 2026 |
| July 31, 2025 | February 26, 2026 |
| August 31, 2025 | March 29, 2026 |
| September 30, 2025 | April 28, 2026 |
| October 31, 2025 | May 29, 2026 |
| November 30, 2025 | June 28, 2026 |
| December 31, 2025 | July 29, 2026 |
| January 31, 2026 | August 29, 2026 |
| February 28, 2026 | September 26, 2026 |
| March 31, 2026 | October 27, 2026 |
| April 30, 2026 | November 26, 2026 |
| May 31, 2026 | December 27, 2026 |
Summary Annual Report (SAR) (Due within 9 months after end of the plan year)
| Plan Year Ending | SAR Due |
| April 30, 2025 | January 31, 2026 |
| May 31, 2025 | February 28, 2026 |
| June 30, 2025 | March 31, 2026 |
| July 31, 2025 | April 30, 2026 |
| August 31, 2025 | May 31, 2026 |
| September 30, 2025 | June 30, 2026 |
| October 31, 2025 | July 31, 2026 |
| November 30, 2025 | August 31, 2026 |
| December 31, 2025 | September 30, 2026 |
| January 31, 2026 | October 31, 2026 |
| February 28, 2026 | November 30, 2026 |
| March 31, 2026 | December 31, 2026 |
FEATURE: Benefits During an Unprotected Leave of Absence
When it comes to administering health plan coverage during an employee’s leave of absence, the first step is to determine whether the employee is entitled to protected leave under federal or state law (e.g., FMLA). For purposes of this summary, an assumption is made that the employee is either not eligible for protected leave or protected leave has already been exhausted.
1. Will an employee who takes unprotected leave remain eligible for health insurance and other benefits?
If an employee enrolled in benefits takes an unprotected leave of absence or exhausts their protected leave, their continued eligibility for benefits during leave will depend on two things: the eligibility rules in the plan documents and the employer’s own leave policies.
Plan Documents
Some plan documents include specific provisions outlining how long an employee on leave may remain covered under the benefit plan before coverage terminates (e.g., plan document may allow eligibility to continue during approved leave for 60 days). When such language exists, the plan document governs. Employers should review all plan documents, including any wrap documents and underlying summary plan descriptions (SPDs) or certificates of coverage, as provisions may differ across benefits.
Employer Leave Policy
In the absence of specific language in the plan documents, it falls on the employer to determine how long an employee on an unprotected leave can remain on the benefit plans as an active participant. Some employers will address eligibility for benefits in the employer’s leave policy or employee handbook. Absent insurance carrier/stop-loss vendor restrictions, employers are free to determine eligibility while on unprotected leave. The employer’s leave policy should establish a definite period of eligibility while on leave (not open-ended), the eligibility should align with any applicable rules within the plan documents, and the employer should apply its policies consistently to all employees. In cases where plan documents and employer policies are vague, silent, or defer to the employer, it is the employer’s responsibility to interpret and apply the information available.
2. When should an employer make an offer of COBRA/continuation coverage to an employee on unprotected leave?
When to offer COBRA/continuation coverage depends on how the plan is administered according to the information in Q-1 above. If, according to the plan terms and/or employer leave policy, the employee’s leave of absence (i.e., reduction in hours) triggers a loss of eligibility for coverage; that triggers a qualifying event requiring the employer to make an offer of COBRA or state continuation coverage.
3. If an employee remains eligible for health coverage during unprotected leave, how should the employer handle premiums?
If the leave of absence is paid, employee contributions may continue to be deducted from payroll. If the leave is unpaid, the employer should have a process for obtaining employee contributions and that process should be communicated to employees. There are no rules that specifically address how employers may collect premiums during unprotected leave, so most employers follow the rules applicable to FMLA by offering at least one of the following options: (1) pre-pay on a pre-tax basis (this cannot be the sole option); (2) pay during the leave on an after-tax basis; or (3) make catch-up contributions on a pre-tax basis upon return from leave. If an employee fails to make their share of premium contributions during the leave in accordance with the employer’s communicated policy, their coverage can be terminated (potentially retroactively). Coverage terminated due to failure to pay premiums is not a COBRA qualifying event.
4. How should the employer handle health plan coverage upon the employee’s return from leave?
13-Week Rule (only applicable large employers (50 or more FTEs))
If an employee returns from unpaid leave within 13 weeks without being credited an hour of service, the employer must treat the employee as a continuing employee. If the employee was previously covered and returned as full-time, the medical coverage must be reinstated as soon as administratively possible (i.e., no later than the 1st of the month following rehire) to avoid potential ACA penalties. If the unpaid leave was longer than 13 weeks, the employee can be treated as a “new hire” upon return and subjected to a new waiting period or initial measurement period, as applicable.
§125 Rules
If the employee returns from unprotected leave within 30 days of coverage being terminated, the employer is required to reinstate the employee’s previous elections (assuming they are eligible upon return). If the leave was longer than 30 days, the cafeteria plan can be designed to reinstate the employee’s prior cafeteria plan election or allow the employee to make a new election to the same extent allowed for new hires.
5. What if the employee takes leave during their waiting period or before medical coverage becomes effective?
HIPAA’s nondiscrimination rules generally prohibit health plans from denying or delaying coverage based on an employee’s ability to work when the absence is health-related. Therefore, for healthrelated leave, coverage should typically become effective once the waiting period is met, even if the employee is not actively at work. If the employee does not return and no longer meets eligibility requirements, coverage may be terminated in accordance with the employer’s standard unprotected leave policies. HIPAA’s nondiscrimination protections apply only to group health plans, not to excepted benefits (e.g., dental/vision coverage, health FSAs) or non-health benefits such as life and disability insurance, which may require the employee to be actively at work before coverage begins.

